Printable Do Not Resuscitate Order Document for Iowa State
Things You Should Know About This Form
-
What is a Do Not Resuscitate (DNR) Order in Iowa?
A Do Not Resuscitate Order is a legal document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. In Iowa, this order specifically instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) if the individual stops breathing or their heart stops beating.
-
Who can create a DNR Order in Iowa?
In Iowa, any adult who is capable of making their own healthcare decisions can create a DNR Order. This includes individuals who are 18 years or older and are able to understand the implications of their choices regarding medical treatment.
-
How do I obtain a DNR Order form in Iowa?
You can obtain a DNR Order form from various sources, including:
- Your healthcare provider or physician's office
- Iowa Department of Public Health website
- Local hospitals or hospice organizations
Ensure that the form is the most current version to meet state requirements.
-
What information is required on the DNR Order form?
The DNR Order form typically requires the following information:
- The patient's name and date of birth
- The signature of the patient or their legal representative
- The signature of a physician or healthcare provider
- Any additional instructions or preferences regarding end-of-life care
-
Is a DNR Order valid in all healthcare settings?
Yes, a properly completed DNR Order is valid in all healthcare settings in Iowa, including hospitals, nursing homes, and at home. However, it is essential to ensure that the order is readily accessible to healthcare providers when needed.
-
Can a DNR Order be revoked or changed?
Absolutely. A DNR Order can be revoked or changed at any time by the individual who created it. This can be done verbally or in writing. It is advisable to inform your healthcare provider and any family members about the changes to ensure everyone is aware of your current wishes.
-
What happens if I do not have a DNR Order?
If you do not have a DNR Order, healthcare providers are required to perform resuscitation efforts if your heart stops or you stop breathing. This may include CPR and other life-saving measures, which may not align with your personal wishes regarding end-of-life care.
-
Will my DNR Order be honored if I travel outside of Iowa?
While many states recognize DNR Orders from other states, it is crucial to check the specific laws of the state you are visiting. Carrying a copy of your DNR Order and any relevant documentation can help ensure that your wishes are respected while traveling.
-
How can I ensure my family understands my DNR wishes?
Communication is key. Discuss your DNR wishes with your family members and loved ones. It may be helpful to provide them with copies of your DNR Order and any related documents. Consider having these conversations early and revisiting them periodically to ensure everyone is on the same page.
-
What resources are available for more information about DNR Orders in Iowa?
For more information about DNR Orders in Iowa, you can consult:
- Your healthcare provider
- The Iowa Department of Public Health website
- Local hospice or palliative care organizations
- Legal resources specializing in healthcare directives
These resources can provide additional guidance and support in understanding DNR Orders and their implications.
File Data
| Fact Name | Details |
|---|---|
| Governing Law | The Iowa Do Not Resuscitate Order is governed by Iowa Code § 144A.2. |
| Eligibility | Any adult with a terminal condition or a serious illness may complete the DNR order. |
| Signature Requirements | The form must be signed by the patient or their legal representative and a physician. |
| Effectiveness | The DNR order is effective statewide and must be honored by all healthcare providers in Iowa. |
Discover Other Common Forms for Iowa
Iowa Trailer Bill of Sale - This document may also be required for inspection before registration at the DMV.
To facilitate a smooth transaction, it's crucial to use the appropriate paperwork when dealing with all-terrain vehicles. The New York ATV Bill of Sale form not only documents the essential details of the sale but also protects the interests of both parties involved. To obtain the necessary document and ensure you meet all legal requirements, you can find the form through PDF Templates.
Non Compete Agreement Iowa - Employees may be offered compensation for signing a Non-compete Agreement.
Iowa Secretary of State Notary - The acknowledgment often includes the date of signing.
Key takeaways
When considering the Iowa Do Not Resuscitate (DNR) Order form, it is essential to understand its purpose and how to properly fill it out. Here are key takeaways to keep in mind:
- The DNR Order is a legal document that informs medical personnel of your wishes regarding resuscitation efforts in case of cardiac or respiratory arrest.
- It must be signed by a physician, and the signature indicates that the physician has discussed the implications of the DNR with you or your legal representative.
- Anyone can request a DNR Order, but it is typically used by individuals with serious health conditions or those nearing the end of life.
- Once completed, the DNR Order should be placed in a prominent location, such as on the refrigerator or with medical records, to ensure it is easily accessible in emergencies.
- It is important to discuss your DNR wishes with family members and healthcare providers to ensure everyone understands your preferences.
- The DNR Order can be revoked at any time. Simply inform your healthcare provider and destroy the original document.
- Keep a copy of the DNR Order for your records, and consider providing copies to family members and your healthcare team.
- Review your DNR Order regularly, especially if your health status changes or if you have new preferences regarding your care.
- Be aware that the DNR Order only applies to resuscitation efforts and does not affect other medical treatments or interventions.
Understanding these key points will help ensure that your wishes are respected and that you receive the appropriate care in line with your preferences.
Sample - Iowa Do Not Resuscitate Order Form
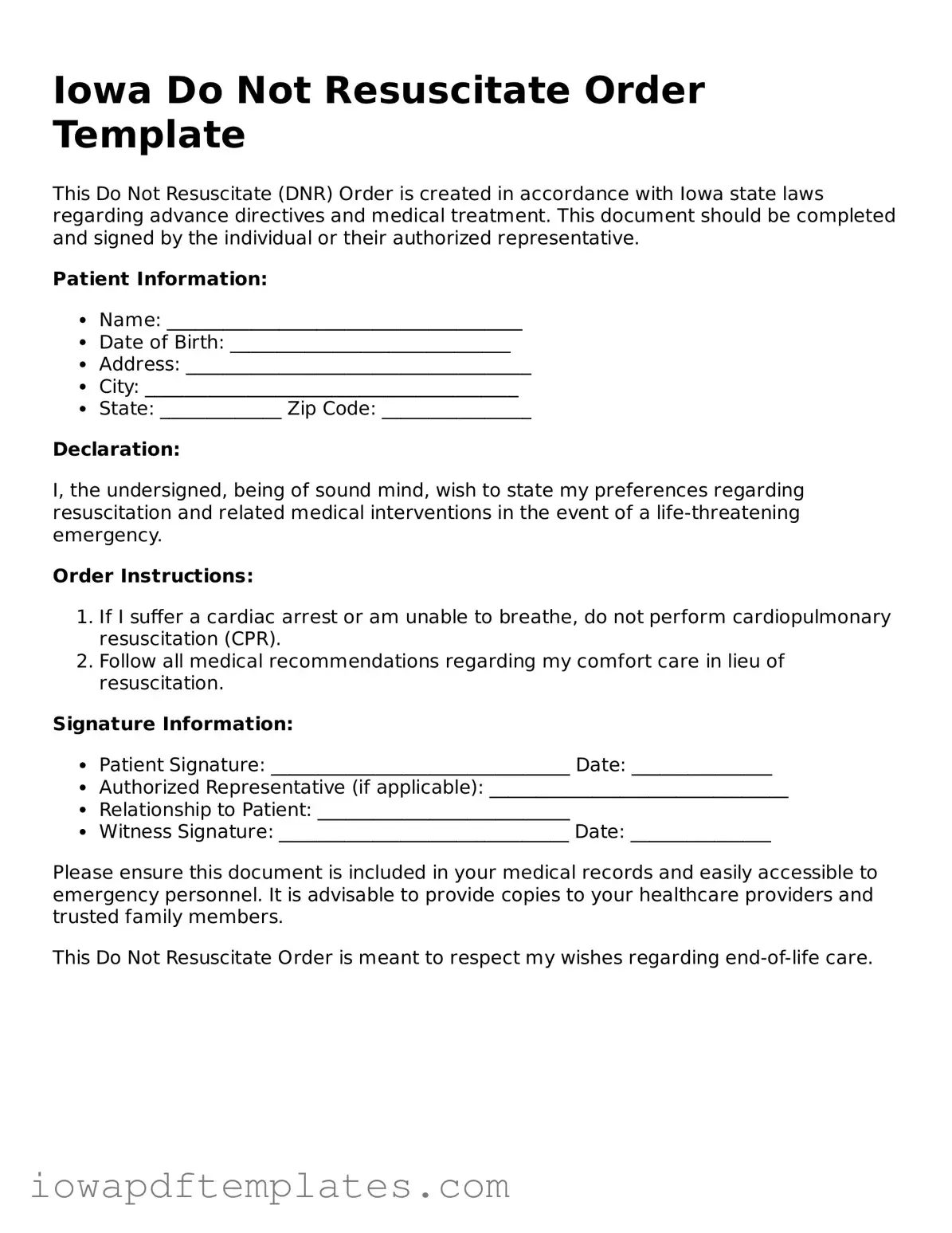
Iowa Do Not Resuscitate Order Template
This Do Not Resuscitate (DNR) Order is created in accordance with Iowa state laws regarding advance directives and medical treatment. This document should be completed and signed by the individual or their authorized representative.
Patient Information:
- Name: ______________________________________
- Date of Birth: ______________________________
- Address: _____________________________________
- City: ________________________________________
- State: _____________ Zip Code: ________________
Declaration:
I, the undersigned, being of sound mind, wish to state my preferences regarding resuscitation and related medical interventions in the event of a life-threatening emergency.
Order Instructions:
- If I suffer a cardiac arrest or am unable to breathe, do not perform cardiopulmonary resuscitation (CPR).
- Follow all medical recommendations regarding my comfort care in lieu of resuscitation.
Signature Information:
- Patient Signature: ________________________________ Date: _______________
- Authorized Representative (if applicable): ________________________________
- Relationship to Patient: ___________________________
- Witness Signature: _______________________________ Date: _______________
Please ensure this document is included in your medical records and easily accessible to emergency personnel. It is advisable to provide copies to your healthcare providers and trusted family members.
This Do Not Resuscitate Order is meant to respect my wishes regarding end-of-life care.
Similar forms
The Iowa Do Not Resuscitate (DNR) Order form shares similarities with the Advance Directive. An Advance Directive is a legal document that outlines a person's wishes regarding medical treatment when they are unable to communicate. Like the DNR, it allows individuals to express their preferences about life-sustaining measures, ensuring that their healthcare aligns with their values and desires. Both documents aim to provide clarity to healthcare providers and family members during critical situations.
Another document akin to the DNR is the Living Will. This legal document specifically details the types of medical treatments a person would or would not want at the end of life. While the DNR focuses on resuscitation efforts, the Living Will can encompass a broader range of medical decisions. Both documents empower individuals to make choices about their medical care, fostering autonomy in healthcare decisions.
The Physician Orders for Life-Sustaining Treatment (POLST) form is also similar to the DNR. POLST is a medical order that reflects a patient’s preferences regarding treatment at the end of life. Unlike the DNR, which primarily addresses resuscitation, POLST can include directives about other interventions, such as feeding tubes or antibiotics. Both documents are intended to communicate a patient’s wishes to healthcare providers, ensuring that those wishes are honored.
Healthcare Power of Attorney (POA) documents share a connection with the DNR as well. A Healthcare POA designates a person to make medical decisions on behalf of someone else if they become incapacitated. While the DNR specifically addresses resuscitation, the Healthcare POA can encompass a wider range of medical decisions. Both documents are crucial for ensuring that an individual's healthcare preferences are respected when they cannot advocate for themselves.
The Comfort Care Order is another document that parallels the DNR. This order focuses on providing comfort and pain relief rather than aggressive medical interventions. While the DNR prevents resuscitation efforts, the Comfort Care Order emphasizes the importance of quality of life in the final stages of life. Both documents reflect a patient’s desire to prioritize comfort over invasive treatments.
Similar to the DNR, the Do Not Intubate (DNI) order specifically addresses a patient’s wishes regarding intubation, a procedure used to assist with breathing. While a DNR prohibits resuscitation efforts, a DNI indicates that a patient does not want to be placed on a ventilator. Both documents are essential for guiding healthcare providers in respecting a patient’s end-of-life wishes.
The Medical Orders for Life-Sustaining Treatment (MOLST) form also resembles the DNR. Like POLST, MOLST serves as a medical order that conveys a patient’s treatment preferences. Both documents aim to ensure that healthcare professionals honor the patient’s choices regarding life-sustaining measures, promoting a patient-centered approach to care.
For those looking to understand the foundational components of their business, a thorough examination of the aspects surrounding the Operating Agreement is crucial. This document not only clarifies management responsibilities but is also pivotal in ensuring operational efficiency. For a more in-depth look, visit key information on the Operating Agreement essentials.
Another related document is the End-of-Life Care Plan. This plan outlines a patient’s preferences for care as they approach the end of life. While the DNR focuses on resuscitation, the End-of-Life Care Plan can cover a range of topics, including pain management and emotional support. Both documents are designed to provide guidance to healthcare providers and loved ones during critical times.
The Palliative Care Plan is similar to the DNR in that it emphasizes comfort and quality of life for patients with serious illnesses. This plan outlines the goals of care, including pain management and symptom relief, rather than aggressive life-saving measures. Both documents reflect a commitment to ensuring that patients receive care aligned with their values and preferences.
Finally, the Hospice Care Agreement shares similarities with the DNR. This agreement is made when a patient chooses to receive hospice care, focusing on comfort and quality of life rather than curative treatments. While the DNR specifically addresses resuscitation, the Hospice Care Agreement encompasses a broader approach to end-of-life care, prioritizing the patient’s wishes and well-being. Both documents aim to provide a clear framework for healthcare decisions during life’s final stages.