Free Iowa 470 0040 Template
Things You Should Know About This Form
What is the Iowa 470 0040 form used for?
The Iowa 470 0040 form is utilized for submitting adjustment requests related to Medicaid claims. It allows providers to request changes or corrections to previously submitted claims. This can include issues such as denied claims, incorrect billing amounts, or necessary updates to patient information.
How do I complete the Iowa 470 0040 form?
To complete the form, follow these steps:
- Identify the reason for your adjustment request in Section A. You must select at least one reason.
- Attach any necessary documentation, such as corrected claims or remittance advice.
- Fill out Section B with essential details, including the 17-digit TCN, NPI number, and patient account number.
- Sign and date the form before submission.
Where should I send the completed Iowa 470 0040 form?
Once you have completed the form, send it to the Iowa Medicaid Enterprise at the following address:
Iowa Medicaid Enterprise
PO Box 36450
Des Moines, IA 50315
What types of adjustments can I request using this form?
You can request various adjustments, including:
- Corrections to diagnosis codes
- Changes to billed amounts
- Adjustments for patient liability
- Updates to procedure codes or modifiers
- Adding new claim details
Ensure that any supporting documentation is included for the requested changes.
What should I avoid when filling out the Iowa 470 0040 form?
When completing the form, avoid using red ink, as it may not be processed correctly. Additionally, ensure that all necessary attachments are included, and double-check for accuracy to prevent delays in processing your request.
How can I download the Iowa 470 0040 form?
The Iowa 470 0040 form can be downloaded from the Iowa Medicaid Enterprise website. Visit this link to access the form and other related documents.
Form Features
| Fact Name | Details |
|---|---|
| Form Purpose | The Iowa 470-0040 form is used to request adjustments for Medicaid claims. |
| Submission Address | Requests must be sent to Iowa Medicaid Enterprise, PO Box 36450, Des Moines, IA 50315. |
| Required Attachments | Each request must include a corrected claim and/or remittance advice, as applicable. |
| Governing Law | This form is governed by the Iowa Administrative Code, specifically Chapter 79 of the Iowa Medicaid program. |
Discover Other PDFs
Iowa Medicaid Card - Information about the financial institution is required.
A Lease Agreement is a legal document that outlines the terms and conditions between a landlord and a tenant regarding the rental of property. It details the rights and responsibilities of each party, helping to prevent misunderstandings and disputes. For a seamless rental experience, consider filling out the Lease Agreement form by clicking the button below. You can also find convenient resources, such as the PDF Templates, to assist in this process.
Rent Reimbursement Form 2022 - The form is part of the state's efforts to assist residents with financial burdens related to housing costs.
Key takeaways
Here are some important points to consider when filling out and using the Iowa 470 0040 form:
- Understand the Purpose: This form is used to request adjustments for Medicaid claims.
- Correct Claims: Always attach the corrected claim and/or remittance advice with your request.
- Denials: If a claim has been denied, you must resubmit it using this form.
- Avoid Red Ink: Make sure to fill out the form in black or blue ink only.
- Specify Changes: Clearly indicate the specific changes or corrections you are requesting in Section A.
- Complete Section B: Fill out all required fields in Section B to ensure your request is processed.
- Use Accurate Information: Double-check the 17-Digit TCN, NPI Number, and other identifiers for accuracy.
- Keep Copies: Always keep a copy of the completed form and any attachments for your records.
- Submit to the Right Address: Send the form to the Iowa Medicaid Enterprise at the specified address.
By following these key points, you can help ensure that your adjustment request is handled smoothly and efficiently.
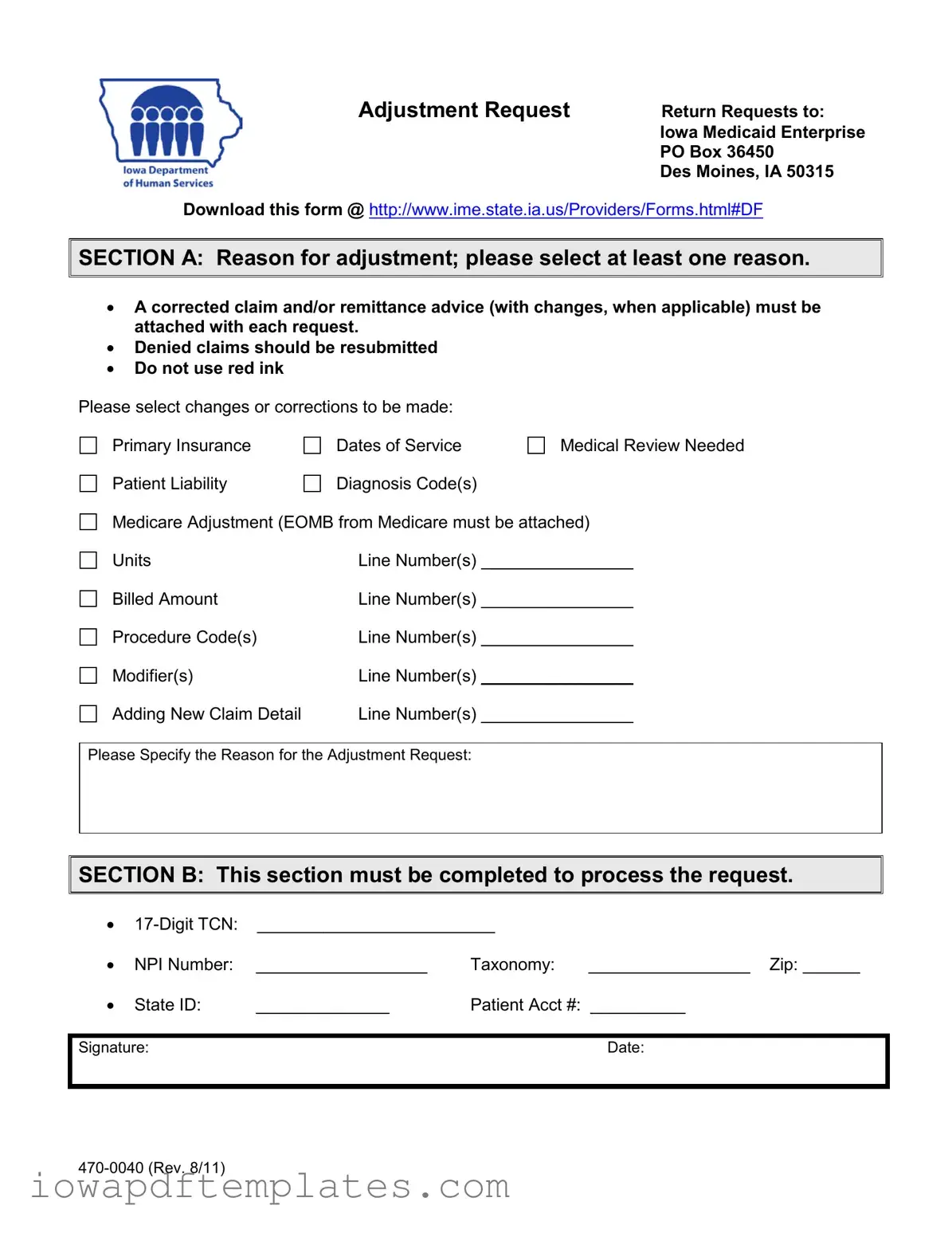
Sample - Iowa 470 0040 Form
Adjustment Request
Return Requests to: Iowa Medicaid Enterprise PO Box 36450
Des Moines, IA 50315
Download this form @ http://www.ime.state.ia.us/Providers/Forms.html#DF


 SECTION A: Reason for adjustment; please select at least one reason.
SECTION A: Reason for adjustment; please select at least one reason.
•A corrected claim and/or remittance advice (with changes, when applicable) must be attached with each request.
•Denied claims should be resubmitted
•Do not use red ink
Please select changes or corrections to be made: |
|
|
Primary Insurance |
Dates of Service |
Medical Review Needed |
Patient Liability |
Diagnosis Code(s) |
|
Medicare Adjustment (EOMB from Medicare must be attached) |
||
Units |
Line Number(s) |
_______________ |
Billed Amount |
Line Number(s) ________________ |
|
Procedure Code(s) |
Line Number(s) ________________ |
|
Modifier(s) |
Line Number(s) ________________ |
|
Adding New Claim Detail |
Line Number(s) ________________ |
|
Please Specify the Reason for the Adjustment Request:


 SECTION B: This section must be completed to process the request.
SECTION B: This section must be completed to process the request.
•
• |
NPI Number: |
__________________ |
Taxonomy: |
_________________ Zip: ______ |
• |
State ID: |
______________ |
Patient Acct #: __________ |
|
|
|
|
|
|
Signature: |
|
|
Date: |
|
|
|
|
|
|
Similar forms
The Iowa 470-0040 form is similar to the CMS-1500 form, which is widely used for billing Medicare and Medicaid services. Both forms allow healthcare providers to submit claims for reimbursement. The CMS-1500 requires detailed patient information, including diagnosis codes and procedure codes, much like the Iowa 470-0040. Each form serves the purpose of ensuring that healthcare providers receive payment for services rendered, while also requiring specific documentation to support claims.
Another document that shares similarities with the Iowa 470-0040 is the UB-04 form. This form is used for institutional claims, such as those submitted by hospitals and nursing facilities. Like the Iowa 470-0040, the UB-04 collects essential information about the patient, services provided, and the reason for the claim. Both forms require providers to attach supporting documentation, ensuring that claims are processed accurately and efficiently.
The Appeal Form is another document akin to the Iowa 470-0040. When a claim is denied, providers often need to submit an appeal to contest the decision. This form typically requires the same information as the Iowa 470-0040, including patient details and the reason for the appeal. Both documents aim to rectify issues with previously submitted claims, allowing providers to seek payment for services rendered.
The Medicare Adjustment Request form is also similar. This form is used specifically for requesting adjustments to Medicare claims. Just as the Iowa 470-0040 allows for corrections to claims, the Medicare Adjustment Request form enables providers to address errors or omissions in their submissions. Both forms ensure that the claims process remains transparent and fair for providers and patients alike.
For individuals seeking to understand essential legal documents, the Durable Power of Attorney form is critical, as it empowers someone to make decisions on behalf of another. You can explore more about the Durable Power of Attorney and its importance in securing your interests at the comprehensive Durable Power of Attorney guide.
The Prior Authorization Request form bears resemblance to the Iowa 470-0040 as well. This document is often required before certain services can be billed to insurance. Like the Iowa 470-0040, it collects detailed information about the patient and the services requested. Both forms help ensure that services are deemed medically necessary before they are provided and billed.
The Claim Reconsideration form is another document that operates similarly to the Iowa 470-0040. When a provider believes a claim was incorrectly processed, they can submit this form to request a review. Both documents require specific information about the claim and the reasons for the reconsideration, facilitating a thorough review process by the payer.
The Coordination of Benefits form shares characteristics with the Iowa 470-0040. This form is used when a patient has multiple insurance policies. It helps determine which insurance should pay first. Like the Iowa 470-0040, it gathers essential information about the patient and their coverage, ensuring that claims are billed correctly and efficiently.
The Medical Necessity Documentation form is also akin to the Iowa 470-0040. This document is often required to support claims for certain services, particularly when they are subject to scrutiny. Both forms require detailed information about the patient's condition and the services provided, helping to justify the need for the services billed.
Finally, the Explanation of Benefits (EOB) form is similar in that it outlines what services were billed and how they were processed by the insurer. While the Iowa 470-0040 is used to request adjustments, the EOB provides feedback on claims that have already been processed. Both documents play a crucial role in the claims process, helping providers understand payment outcomes and necessary adjustments.